Fungal toenail infections, medically known as onychomycosis, are common yet often misunderstood. People often suffer additional discomfort due to misconceptions and myths about these infections.
Possible treatments range from over the counter (OTC) antifungal creams and ointments, oral antifungal drugs, and even laser therapy.
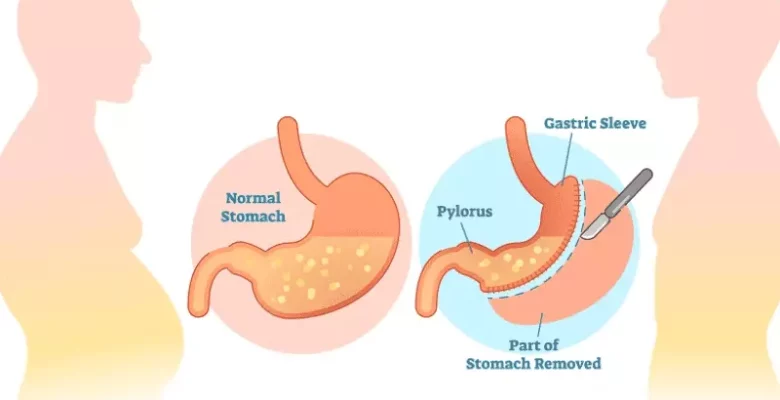
Doctors sometimes debride the nail, which involves removing part of the infected nail to reduce pain and allow topical treatments to work more effectively. For more information about possible treatments, you may wish to visit Anytime Doctor (anytimedoctor.co.uk).
Now let’s look at – and debunk – two myths about fungal toenail infections.
Myth: poor hygiene is the only cause of fungal toenail infections
A widespread myth about fungal toenail infections is that they result solely from poor hygiene. While good hygiene can help prevent infections, it’s not the only contributing factor.
The reality is more complex. Fungal toenail infections are caused by dermatophytes (a type of fungi), yeasts, and moulds. These microorganisms thrive in warm, moist environments, which makes places like public showers, swimming pools, and locker rooms ideal breeding grounds.
A person won’t necessarily develop an infection if exposed to these potential causes. The chance of an infection increases with prolonged exposure, minor injuries to the nail, and certain predisposing factors.
For instance, wearing tight-fitting shoes or having sweaty feet makes an infection likelier. Activities like walking barefoot in communal areas increase the likelihood of contact with fungal spores.
People with compromised immune systems, diabetes, or circulatory issues are more susceptible to infections.
Genetics also play a role in susceptibility. Some people are more predisposed to infections, making them likelier to develop fungal toenails despite good hygiene practices.
Age is also a risk factor, as blood flow to our nails decreases as we age, and nails grow more slowly and thicken, creating more surface area for fungi to inhabit.
Maintaining clean and dry feet is crucial for prevention; however, it does not entirely eliminate the risk.
Myth: OTC treatments always solve the problem
Some people believe that OTC treatments will always cure fungal toenail infections. While these treatments can be helpful for some, they are not universally effective.
Fungal toenail infections can be difficult to treat due to the nature of the infection and the structure of the toenail. Fungi reside not just on the surface but also underneath the nail, making it hard for topical treatments to reach the infection.
OTC antifungal creams, ointments, and nail lacquers are available and can be effective for mild cases. However, they often fail to penetrate the nail sufficiently to get rid of a more severe infection.
More severe infections can require stronger prescription medications. Oral antifungal drugs such as terbinafine and itraconazole are sometimes prescribed and can be more effective than topical treatments.
These medications work by helping a new, healthy nail grow, gradually replacing the infected nail. However, they may need to be taken for several weeks to months, and they come with potential side effects and interactions with other medications.
A final word
Understanding the realities behind these myths can help people take more effective measures to prevent and treat fungal toenail infections. By acknowledging the multifactorial nature of toenail infections and the limitations of OTC treatments, individuals can seek the best care and better manage this frustrating condition.